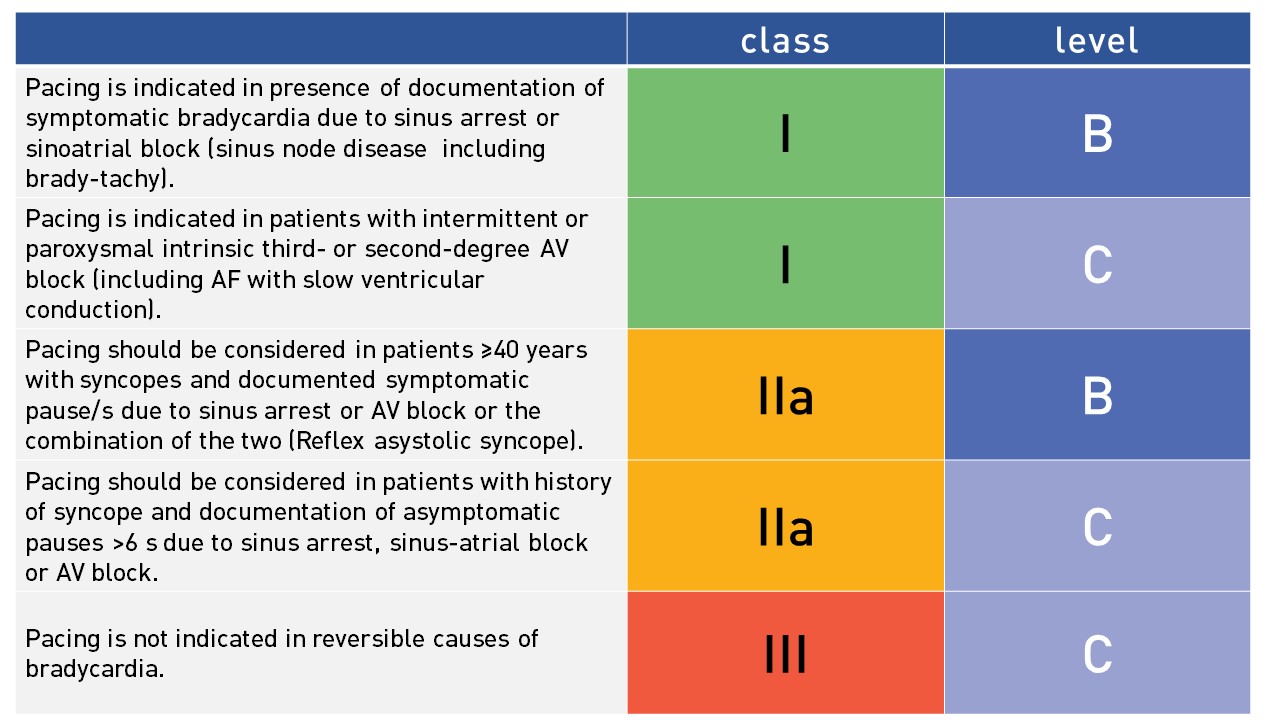
When the correlation between symptoms and documented bradycardia is established, cardiac pacing is considered effective and useful for symptom relief. In the absence of such correlation, the mechanism of undocumented intermittent symptoms (e.g. syncope) in patients with permanent mild sinusbradycardie (i.e. 40–50 bpm) itself asymptomatic, remains uncertain as other competitive causes such as disturbance of the autonomic nervous system often play an important role.
Pacing is indicated in patients with sick sinus node disease (including brady-tachy form) with documentation of symptomatic bradycardia due to sinus arrest or sinusatrial block (I B recommendation). Pacing is also indicated in patients with intermittent/paroxysmal intrinsic third- or seconddegree AV block (I C recommendation). Pacing should be considered in patients with history of syncope and documentation of asymptomatic pauses >6 s due to sinus arrest, sinus-atrial block or AV block. In the patients correlation is less important than in sinus node disease, because there is general consensus that pacing prevents recurrence of syncope and may improve survival. Pacing should be considered in patients ≥40 years with syncopes and documented symptomatic pause/s due to sinus arrest or AV block or the combination of the two.
Adjusted table from the ESC guideline on intermittent bradycardia
Suspected bradycardia
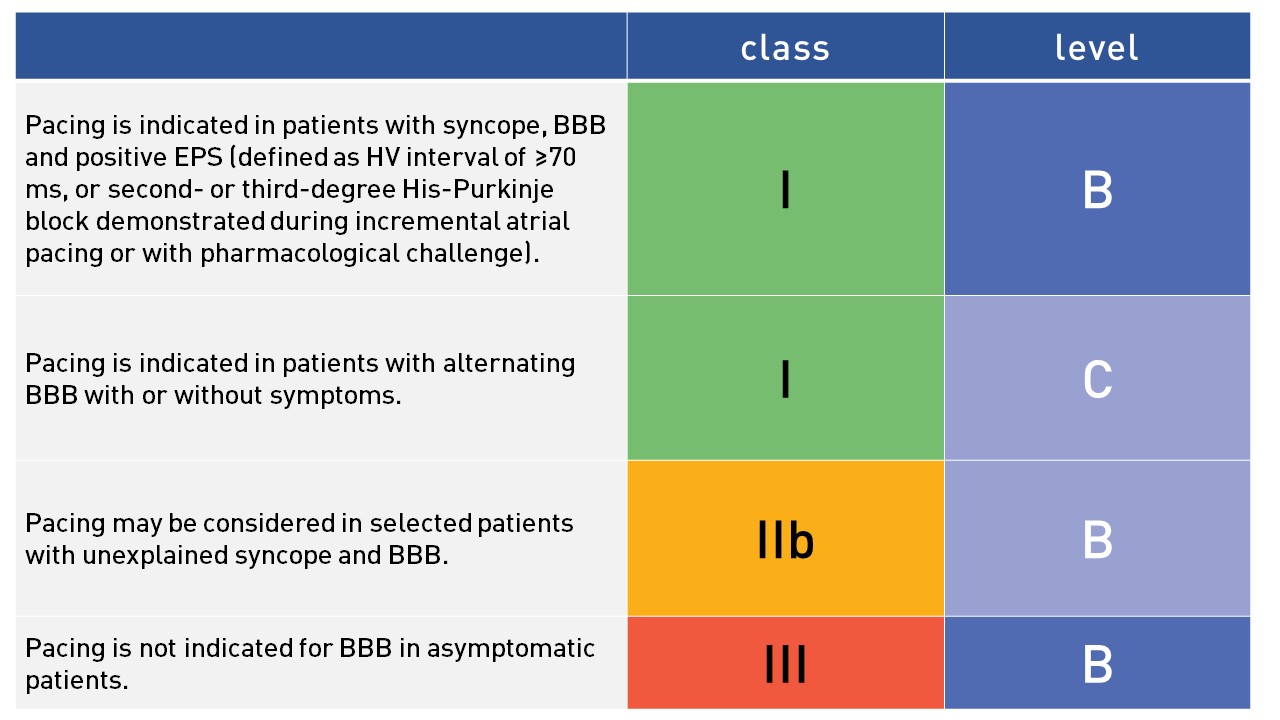
In patients with syncope, the presence of a bundle branch block suggests that the cause of syncope may be complete heart block. Carotid sinus massage and implantion of an internal loop recorder may facilitate a final diagnosis. Electrophysiological investigation including measurement of the HV-interval may aid in decision making. However, the benefit should be weighed against the risk and cost of an invasive procedure. There is a strong consensus that patients with alternating bundle branch block will benefit from cardiac pacing (I C recommendation). In symptomatic patients with left bundle branch block and/or sufficiently broad QRS with severe systolic left ventricular (LV) dysfunction an cardiac resynchronization therapy with or without defibrillator should be considered instead of a pacemaker.
Adjusted table from the ESC guidelines on bundle branch block
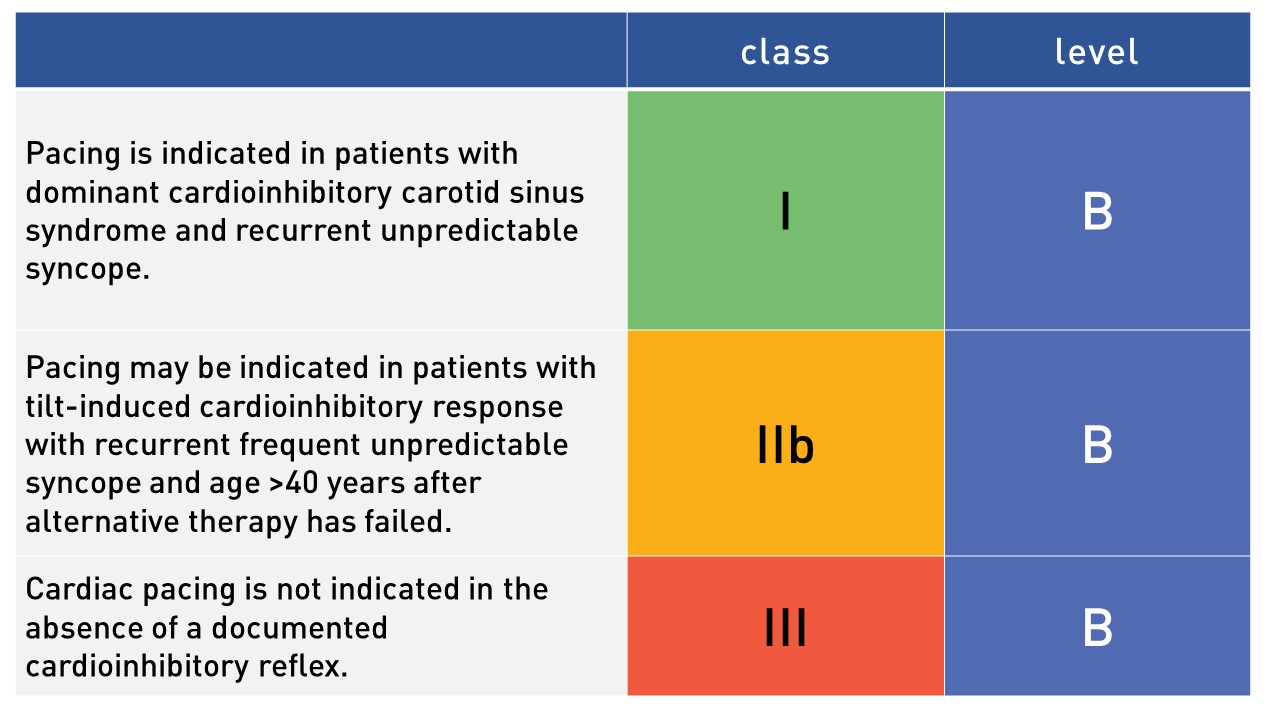
Pacing is indicated in patients with dominant cardioinhibitory carotid sinus syndrome and recurrent unpredictable syncope (I B). For the diagnosis a full 10 sec of massage is required; massage is to be performed supine and erect and pacing (dual chamber) is indicated when .6 sec asystole occurs with reproduction of syncope.
In patients with reflex syncope indication for pacing is highly disputable and divergence of opinion exists among experts, The fact that pacing may be effective does not mean that it is also always necessary. It must be emphasized that the decision to implant a pacemaker needs to be made in the clinical context of a benign condition that frequently affects young patients. Thus, cardiac pacing should be limited, as a last resort choice, to a highly selected small proportion of patients affected by severe reflex syncope. Patients suitable for cardiac pacing are probably those >60 years with a history of recurrent syncope beginning in middle or older ages and with frequent injuries, probably due to presentation without warning. Pacing may be indicated in patients with tilt-induced cardioinhibitory response with recurrent frequent unpredictable syncope and age >40 years after alternative therapy has failed.
Adjusted table from the ESC guideline: