Real-time EGM
Case Summary
0 of 1 Questions completed
Questions:
Information
You have already completed the case before. Hence you can not start it again.
Case is loading…
You must sign in or sign up to start the case.
You must first complete the following:
Results
Results
Time has elapsed
Catégories
- Pas classé 0%
-
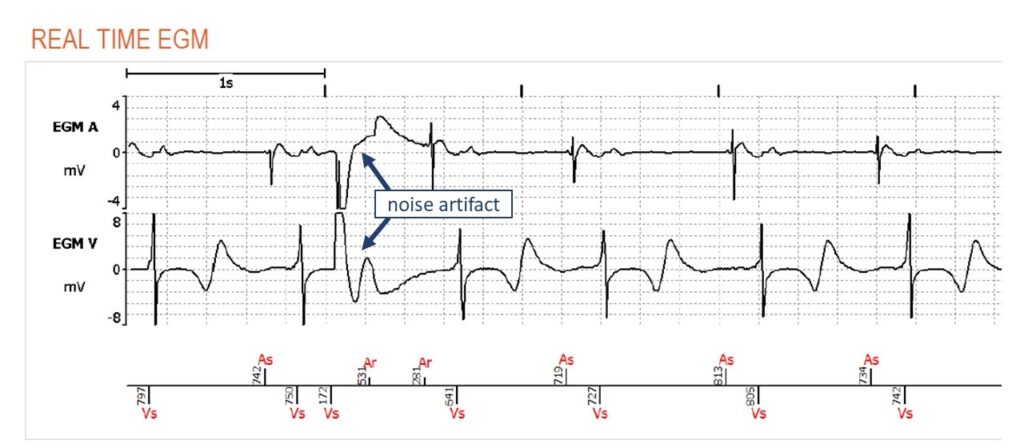
While the transmission does not display any alerts, examination of the real time EGM raises the suspicion of lead noise.
Transmission
The real time EGM is a seven-second registration of the atrial and ventricular EGM at the time of the transmission. In this case, we see atrial and ventricular sensed events, corresponding to a normal sinus rhythm during SafeR mode. Suddenly, after the second ventricular beat, we observe a sudden disruption of the ventricular and atrial signal, which is sensed on both channels. The EGM is distorted, clipped and not compatible with normal physiology. While the noise artifact on the ventricular EGM may resemble a premature ventricular complex, there is no compensatory pause and it would not explain the noise event on the atrial channel at the exact same moment. Simultaneous noise artifacts on both channels is mostly caused by concomitant insulation breach of both leads. As the leads are interacting with each other, mostly within the pocket, the resulting mechanical friction causes the lead noise.
Evaluation of risk
In order to evaluate the risk of an implanted patient with signs of lead failure on remote monitoring, a few high risk factors need to be excluded. The EGM showing sinus rhythm and low % RV pacing burden reveal that the patient is not pacemaker dependant. Signs of RV lead dysfunction in a pacemaker dependant patient is considered a medical emergency. If this were to be an ICD patient, it would also greatly increase the risk of clinical complications as there is a chance of inappropriate therapies.
Analysis of the transmission reveals that lead measurements are within normal range with stable impedances, thresholds and sensing parameters. Unfortunately, the first signs of lead failure are often only visual on the EGM, and these are difficult for the device to detect. While some ICDs have dedicated noise detecting algorithms, pacemakers do not, and we are reliant on real time EGMs or EGMs which were registered due to suspicion of arrhythmia (nonsustained ventricular tachycardia) or activation of an algorithm. In this case, there are signs of early lead failure in a patient with low risk for syncope. Therefore, it is not a medical emergency in which the patient should be advised to come into the device clinic without driving a car. It remains however, an indication to come into clinic for further lead testing.
Next steps
Clinical evaluation of the patient is important to confirm the diagnosis of lead failure. The running EGM may show new noise artifacts, especially during noise exacerbation maneuvres. Mouvement of the arm, breathing exercises and pocket manipulation should be performed to reveal new artifacts. A chest X-ray may reveal lead issues and serve as a reference for a new intervention. In most cases, it will be decided to change the leads in order to ensure the patient’s safety. It is not recommended to decrease device sensitivity or program asynchronous modes or modes with triggering on the long term. It is also important to alert the implanting physician of the complication as certain techniques are associated with higher risk of lead failure such as subclavian puncture which results in risk of subclavian crush syndrome.
- 1
- Current
- Review / Skip
- Answered
- Exact
- Inexact
-
Question 1 of 1
1. Question
You receive the following transmission from a patient implanted with a dual chamber pacemaker due to paroxysmal 2-to-1 block one year prior.
There is no alert within the transmission. What is the most probable diagnosis?
ExactInexact