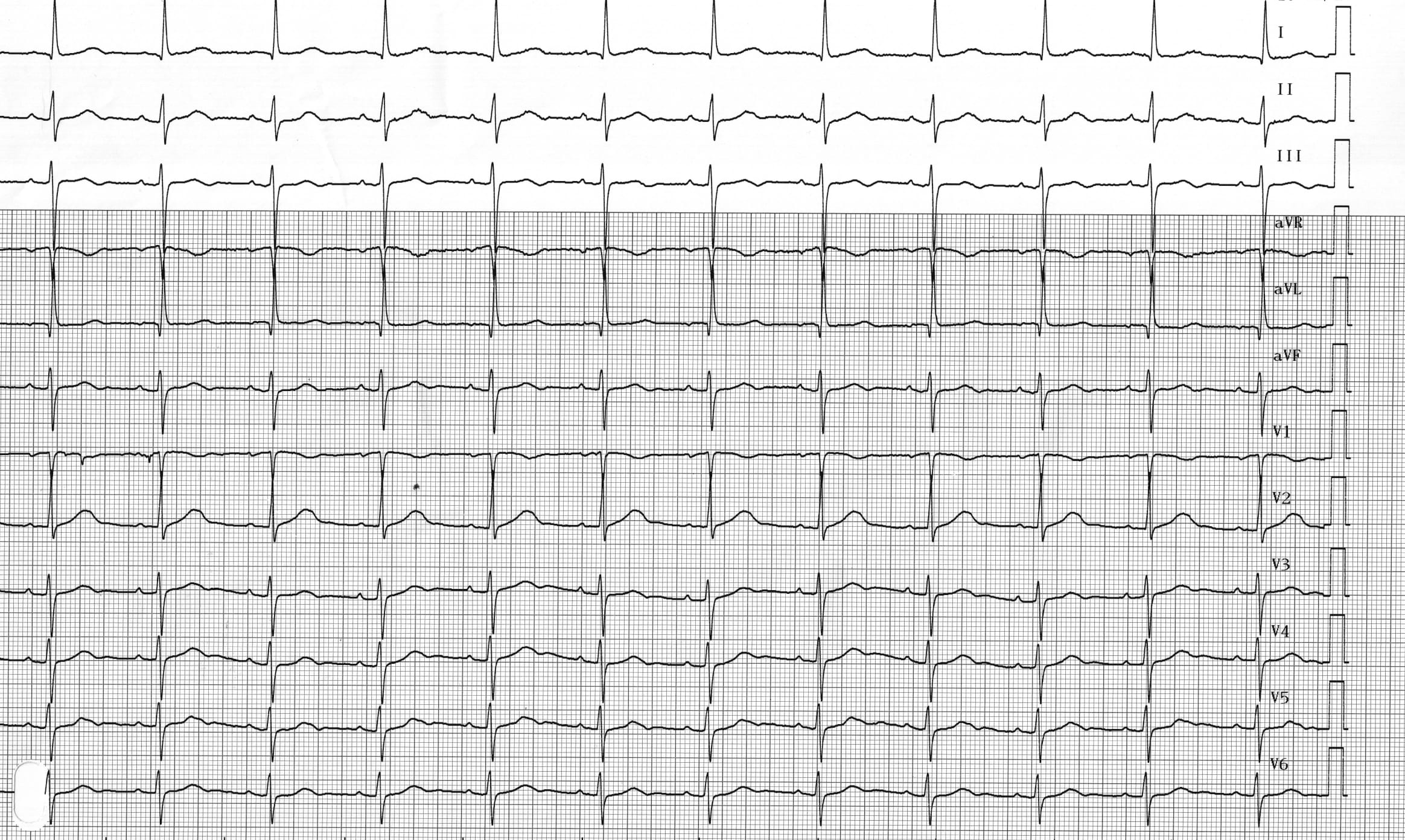
Patient: 69-year-old man implanted with a Medtronic dual-chamber pacemaker following repeated syncopes due to sinus node dysfunction; the 2 pacing leads are well positioned with normal pacing impedances, correct sensing and satisfactory pacing thresholds; 3 days after implantation, pacemaker evaluation; programming of various pacing modes and recording of tracings; for this first tracing, device programmed to ODO mode;
Case Summary
0 of 1 Questions completed
Questions:
Information
You have already completed the case before. Hence you can not start it again.
Case is loading…
You must sign in or sign up to start the case.
You must first complete the following:
Results
Results
0 of 1 Questions answered correctly
Time has elapsed
Categories
- Not categorized 0%
-
ODO mode
ECG 1A: Spontaneous atria and sinus rhythm (positive P waves in leads I, II, V5, V6, negative in aVR); fixed and normal PR interval (< 200 ms); spontaneous ventricles with left anterior fascicular block pattern (left axis, q1S3 pattern);
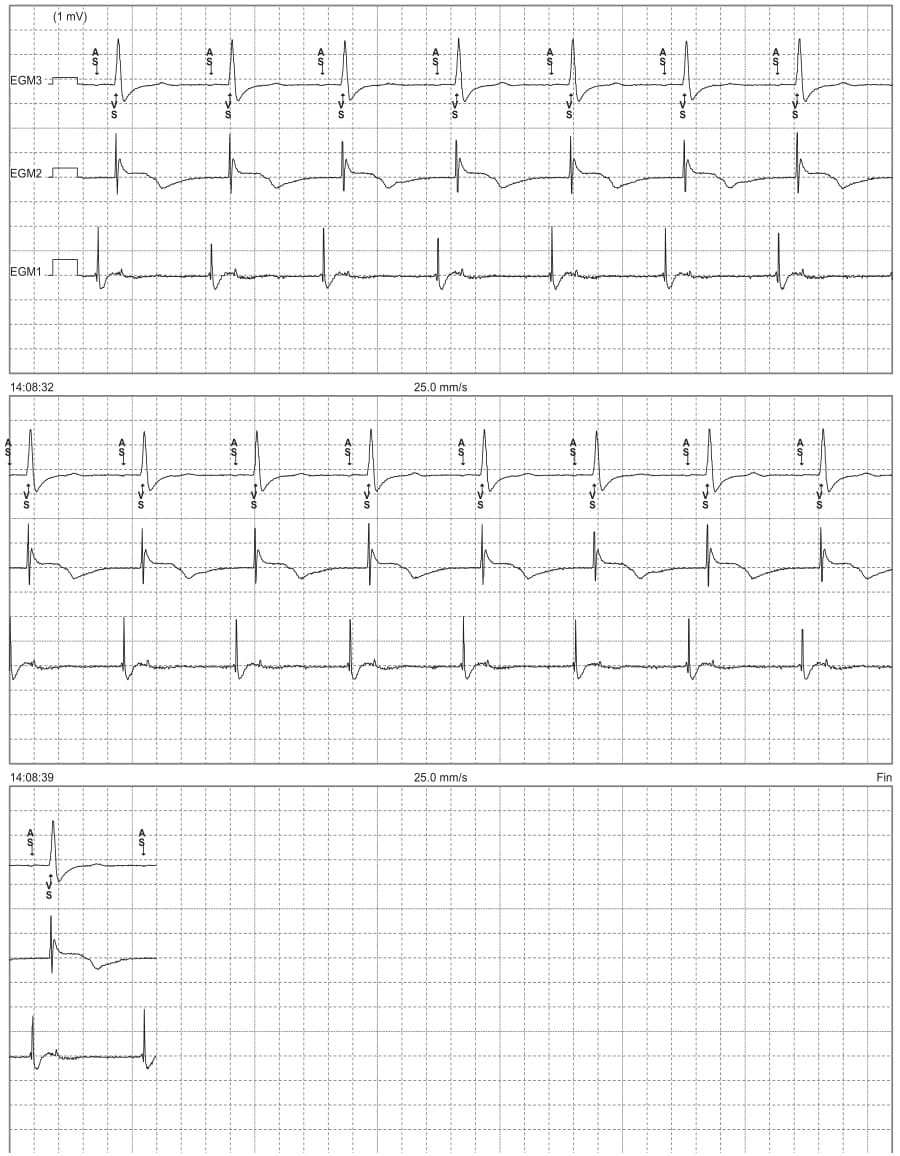
ECG 1B: This is the recording (simultaneously with the previous tracing) of the endocavitary electrograms (EGM) from the programmer; EGM 3 corresponds to an electrocardiographic lead, EGM2 to the ventricular EGM and EGM1 to the atrial EGM; spontaneous atrial and ventricular activities (AS-VS);
Comments: Depending on the number of leads and the implanted device model, various pacing modes are programmable. The functional operation, advantages and disadvantages associated with each pacing mode must be understood by the physician responsible for the follow-up to optimize the programming in conjunction with the specific characteristics of the various device recipients. A combined approach between the North American Society of Pacing and Electrophysiology and the British Pacing and Electrophysiology Group (NASPE and BPEG) has allowed defining an international code (NBG) for the classification of the different pacing modes. The various pacing modes are assigned a 4-letter code that describes their basic functioning. The first letter defines the pacing site(s): ventricle (V), atrium (A), both (D), single chamber (S) or none (O). The second letter defines the sensing site(s): same letters. The third letter indicates the pacing mode: inhibited (I), triggered (T), both (D), none of the previous (O). The fourth letter indicates the rate response (R) or its absence (O).
On this first tracing, the pacemaker was programmed to ODO mode. The specificity of this mode of “pacing” is that there is effective sensing in both cavities but no pacing (atrial or ventricular) is possible. It is obviously to be avoided in pacemaker-dependent patients. This pacing mode therefore allows an analysis of the spontaneous rhythm of the patient with a concomitant visualization of the electrocardiogram and event markers. This is a sensitivity test mode. The ODO mode can be programmed temporarily in non-dependent patients with an MRI-compatible pacemaker who need to undergo an MRI. The ODO mode of these compatible MRI pacemakers prevents the possible reversion from a traditional ODO mode to a VVI mode. Obviously, it is important not to forget to interrogate and reprogram the pacemaker after the examination (according to the various manufacturers).
Take-home message: In a dual-chamber pacemaker, there are different programmable modes, each with its respective specificities; DOO mode: no possibility of sensing, asynchronous pacing; ODO mode: no pacing; DDT mode: trigger mode, sensing triggers pacing; VDD mode: absence of atrial pacing; DDI mode: absence of ventricular pacing following an atrial sensing; DDD mode: ventricular synchronization upon atrial sensing and ventricular pacing; modes are specific to each manufacturer to avoid unnecessary ventricular pacing;
- 1
- Current
- Review
- Answered
- Correct
- Incorrect
-
Question 1 of 1
1. Question
Regarding this ECG, which answer(s) is(are) true?
CorrectIncorrect