Benefits of remote monitoring of PMs
Although remote monitoring (RM) of implanted cardioverter defibrillators (ICDs) is considered essential, it is not always the same for pacemakers. A 2014 European survey including 54 centers revealed that ICD remote monitoring was regarded to be of high or medium benefit for management of ICDs by 94% of the centers while 86% found RM to be of only medium/small benefit or no benefit at all for pacemakers and >80% reported to not perform pacemaker RM.
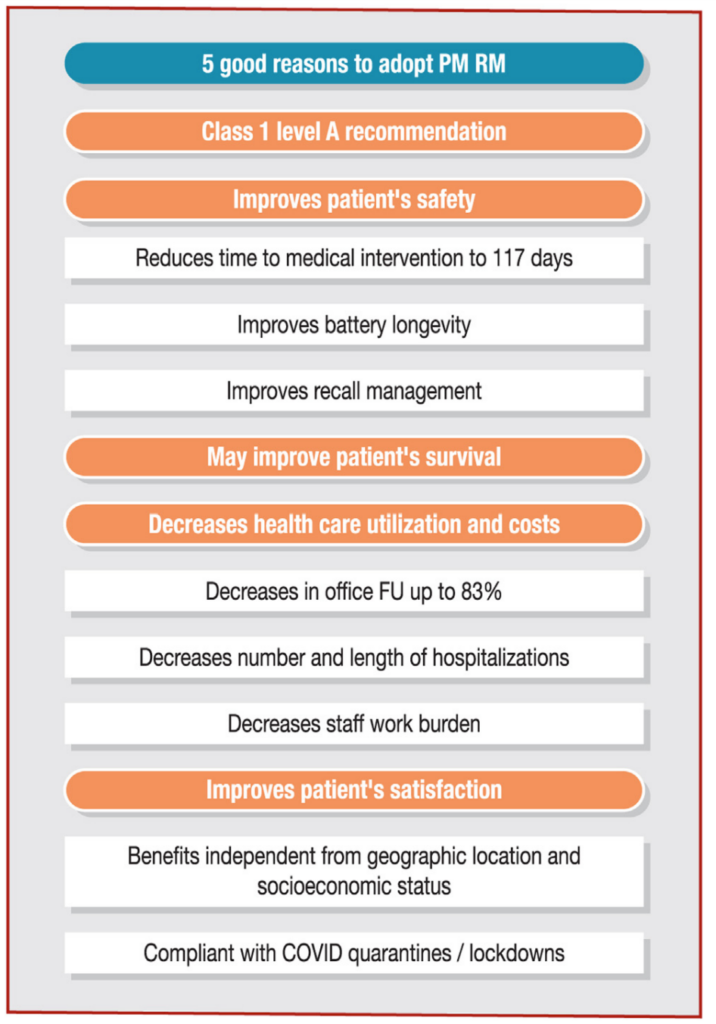
Five good reasons to adopt pacemaker (PM) remote
monitoring (RM). COVID: coronavirus disease 2019; FU: follow-up.
Technical considerations
Remote follow-up solely based on active scheduled patient-activated transmissions have now been abandoned by all pacemaker manufacturers. Contemporary remote monitoring of pacemakers is now similar to ICDs, meaning an automatic driven transmission system based on alerts. Today, all pacemaker manufacturers deliver pacemakers with automatic transmissions. Transmissions are initiated at scheduled intervals with additional alerts for pre-specified out of range parameters. Proprietary transceivers using radiofrequency tend to be progressively replaced by smartphones which communicate with the implanted device through Bluetooth. This later strategy is considered more secure and allows the patient to access a limited amount of information about the pacemaker (mostly battery status) and RM status (date of the next scheduled transmission and past successful transmissions) through use of an app. Compared to bedside transceivers, the use of such app is associated with a greater adherence to transmission schedule. However, the Bluetooth™ communication has a superior energy cost for both smartphone and pacemaker and Bluetooth should be deactivated on pacemakers that are not under RM. Nowadays, most of the pacemakers have auto testing features that allow complete surveillance of the leads and battery. Technical alerts such as lead impedance issue usually require the device to be interrogated by a programmer in order to re-enable the alert transmission. Pacemakers are able to send a various amount of arrhythmic EGM per session and between two programmer interrogations. Additional “real time” EGMs are sent along with periodic remote interrogations. These EGMs enable the identification of pacing/sensing issues. In addition, unscheduled interrogation can be initiated by the patient on most of the systems.
Security/Early detection of events
Owing to the fact that the CIED remote monitoring technology is becoming more and more similar for pacemakers and ICDs, patients implanted with pacemakers also benefit from early detection capabilities of automatic RM. This means that clinical events (such as atrial or ventricular arrhythmia) and technical events (such as signs of lead dysfunction or an empty battery) may be detected and acted upon before the onset of symptoms. In the COMPAS randomized trial (COMPArative follow-up Schedule with home monitoring) the median delay in medical intervention was 17 days in the RM group versus 139 days in the control group, corresponding to a mean gain of 117 days. In a worldwide proprietary database which included 4,631 patients under RM the estimated temporal gain in detection of asymptomatic events (clinical or technical) was 154 days.
Atrial fibrillation (AF) episodes account for the vast majority of events. These notifications may permit early treatment strategies for this largely asymptomatic problem. The SETAM (Strategy of Early Detection of Atrial Arrhythmias with Home Monitoring) randomized trial showed that RM reduces the time to treatment of atrial fibrillation by 44%. After a mean follow-up of 12.8 ± 3.3 months, the AF burden was decreased in the RM arm (8 ± 26% versus 28 ± 43%/day; p=0.04). The importance of AF episodes <24h for risk stratification was shown in the ASSERT trial. Recently NOAH AFNET and ARTESIA were finally published, two large randomized clinical trials which investigated the safety and efficacy of NOAC after episodes of AF. A meta-analysis of these two studies report a reduction in stroke at the price of more bleeds (mostly requiring no intervention. More about this in another, more dedicated lesson.
Regarding device function, RM management improves battery longevity of pacemakers similarly to ICDs When pacemaker safety notification are released regarding a potential device malfunction which could lead to loss of ventricular pacing or battery depletion, remote monitoring is often advised.
Mortality benefit
There are no randomized trials which have demonstrated the survival benefit of RM for pacemakers. However, this question was addressed in a mega-cohort observational study which included 269471 patients of whom 115076 were pacemaker recipients. This study not only showed that RM was associated with improved survival but also that the degree of adherence to remote management correlated strikingly with the magnitude of survival gain. As shown in the Figure, the effect was similarly observed in ICDs and pacemakers. In this study, the clinical profiles beyond age and sex were unavailable but the similar effects of RM observed in both pacemakers and ICDs suggest that the underlying cardiomyopathy does not play an important role.
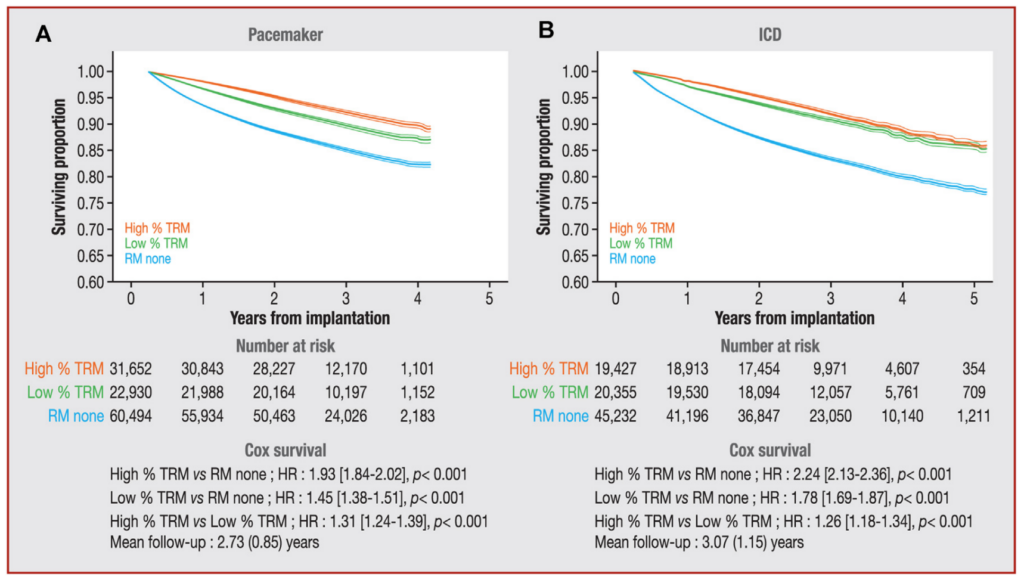 Survival curves of pacemaker recipients versus implantable cardioverter defibrillator (ICD) recipients under remote monitoring (RM). A and B. High percentage of time in RM (%TRM; orange line) consistently had higher survival curves compared with low %TRM (green line) and RM None (blue line) for both pacemakers (A) and ICDs (B). HR: hazard ratio. Reproduced from Varma et al., 2014
Survival curves of pacemaker recipients versus implantable cardioverter defibrillator (ICD) recipients under remote monitoring (RM). A and B. High percentage of time in RM (%TRM; orange line) consistently had higher survival curves compared with low %TRM (green line) and RM None (blue line) for both pacemakers (A) and ICDs (B). HR: hazard ratio. Reproduced from Varma et al., 2014
Although socioeconomic factors (estimated from the ZIP codes) significantly affected connectivity, the magnitude of the association was insubstantial and insufficient to explain the results. Survival data from the same cohort also indicate that when compared with delayed initiation (after 3 months), prompt initiation of pacemaker RM was associated with a greater adjusted survival (HR 1.19 [95 % CI 1.12–1.27], p < 0.001).[18] The survival benefit observed with pacemaker RM is probably multifactorial. Early interventions on atrial arrhythmias, ventricular high-rate episodes (either due to sinus tachycardia, AF or VT), and lead/device malfunctions may translate in better outcomes. Illustrative cases of actionable alerts that may have changed the prognoses of the patients are depicted in Figures 1, 3, 4 and 5. Patient contacts prompted by RM (or interruption of RM) may occasionally reveal worsening of their clinical status. It has been postulated that use of RM may be more likely in patients who are generally healthier and more compliant. However it has been shown that patients randomized to RM are less likely to be lost to follow-up and more likely to adhere to in-person follow-up.[19] Finally, intensified follow-up may improve health conscious behaviour beyond device management.
Health care utilization and costs
Pacemakers remote monitoring diminishes the need of interim follow-ups, which are known to not require programming changes in 79-99% of cases. The randomized COMPAS trial first showed that automatic RM was a safe alternative to conventional long term follow-up over an 18 months period. Among other benefits, RM provided a 36% reduction in the number of follow-up per patient. The RM Alone study showed, that is safe to replace in office interrogations by periodic remote interrogations in a randomized population of 294 pacemaker recipients followed by automatic remote monitoring for at least 24 months. The proportion of patients experiencing ≥1 major cardiac event was similar between the two groups, but remote interrogations was associated with a 83% reduction in face-to-face visits and a significant decrease in the staff workload. The same design was applied in the At-Home Study which included 1274 patients. After 24 months, the absence of in-office scheduled interrogations provided a 70% reduction of in-office follow-ups without an increase in major cardiac events. In none of these trials, the rate of hospitalization was significantly different between groups.
Remote monitoring is also a useful strategy to limit the time spent in hospitalization. In the OnE Day pacemaker Implantation Program with homE-monitoring (OEDIPE) trial, RM was used to enable early hospital discharge after pacemaker implant or replacement. The use of RM was shown to be safe and provided a 34% reduction in the mean hospital duration (p<0.001). Piccini et al assessed the health care utilization in a US nationwide cohort study which included 54520 pacemaker recipients of whom 15571 were remotely monitored. The use of RM (either active or automatic) was associated with a reduced risk (adjusted for geography, age, sex, and 20 pre-implant comorbidities) of all-cause hospitalization (HR: 0.83 [95%CI: 0.81-0.86], p<0.001 and CV hospitalization HR: 0.86 [95%CI: 0.82-0.91], p<0.001). The number of days spent per year was also reduced from 3.3 d/pt/y to 2.1d/pt/y under RM (p<0.001). As a result, RM was associated with a 31% lower hospitalization costs (p<0.001). Interestingly these results were similar to those observed in the 27816 ICD recipients included in the same study.
Conclusions
However, the perception still exists among many that RM of pacemaker is non-essential, despite the very similar gains that are achieved compared to ICD RM. The reductions of in-office evaluation and in the overall staff workload are important when these resources are stretched to their limits. The early detection ability provided by RM facilitates device management (extending battery longevity) and ability to exercise vigilance over recalled components. RM reduces similarly the risk of all-cause hospitalization and death for both pacemaker and ICD devices in a mega-cohort observational study. It is anticipated that RM will be an important ingredient to anticoagulation decisions for AF. When available, the reimbursement is independent of the device type. Finally, pacemakers benefit from the same Class I Level A recommendation as ICDs. These extensive benefits indicate that RM should not be denied to pacemaker recipients.