Benefits of remote monitoring of ICDs
In recent years, especially during the ongoing coronavirus pandemic, remote monitoring (RM) for implantable cardioverter defibrillators (ICDs) has become increasingly popular and accepted. Its use has spread more and more. The benefits are multiple and well established for both ICD and pacemakers. In this lesson we discuss the most important aspects of RM in ICDs.
While remote monitoring of patients implanted with an ICD is considered a “no-brainer” by most, there is still an unacceptable amount of patients not receiving this service. This is mostly due to organizational and financial constraints.
Detection of lead or generator issues
The essential function of an ICD system depends on its sensing and defibrillation capabilities. These functions rely on lead integrity which is known to be the weakest part in all ICD systems. Lead failure may lead to loss of bradycardia pacing, missed treatment of ventricular arrhythmias (ATP or defibrillation) or to inappropriate therapies caused by oversensing. Inappropriate shocks decrease the quality of life and the life expectancy of the ICD recipient. Most ICDs today have the ability to send data automatically in cases of device malfunction. In the TRUST trial, ICD patients were randomized to RM with daily transmissions or to conventional care with in-office visit only. Lead and generator problems were detected significantly earlier in the RM group compared to the conventional care group (median of 1 vs. 5 days, respectively; p=0.05). Recently, most of the manufacturers of implantable cardiac devices faced problems with lithium plating which randomly can cause rapid battery depletion. Here, activating RM was strictly recommended by the manufacturers and became a beneficial and irreplaceable instrument for both patient and healthcare professional helping to detect affected devices as early as possible. All ICDs are equipped with alerts based on impedance abnormalities which is highly specific for detecting lead failure, while the sensivity of this approach is limited. Therefore, certain ICDs have specific noise-detection algorithms mostly based on sensing fast events on the near field channel or lack thereof on the far field channel. Therefore, all experts agree that RM is very important for ICD recipients even though in many centers it is not performed for all candidates due to planning and reimbursement issues.
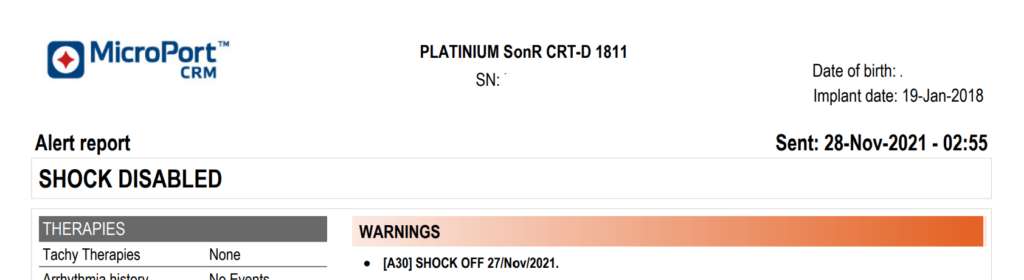
Example of an ICD related alert. The patient underwent MRI scanning (therapies switched OFF) and inadvertently the therapies were not switched back ON. The ICD sent an alert reminding the remote monitoring team that the shocks were disabled. The patient was asked to come back into clinic to switch ON the therapies.
While less critical than ICD RV lead failure, a right atrial or left ventricular lead malfunction may have clinical consequences. A right atrial lead malfunction may favor pacemaker mediated tachycardia, loss of cardiac resynchronization therapy (CRT) or SVT-VT discrimination errors.
Detection of Cardiac Arrhythmias
Whenever sustained ventricular tachycardia occurs, it is essential to check whether the ICD has properly and timely diagnosed the arrhythmia and that treatment was performed correctly and efficiently. Timely transmission of treated or non-treated ventricular episodes is important to facilitate intervention by the remote monitoring team to prevent future inappropatie therapies or lack of appropriate therapies. Shocks delivered by an ICD are often not noticed by the patient and RM can lead to changes in medical treatment including invasive ablation which aim to prevent future shocks. Even more so for antitachycardia pacing (ATP), these often asymptomatic episodes are a true target for RM as diagnostic or therapeutic interventions can decrease recurrence. Boulé et al. demonstrated that RM systems that generate alerts following ATP delivery could reduce emergency presentations for ICD shock by 24%. In addition, non-shocked VT and VF episodes may relate to supraventricular tachycardia, P/R/T-wave oversensing, noise oversensing or lead dysfunction. We know also that the nonsustained ventricular arrhythmias, commonly transmitted with RM, are often discarded while they are associated with a five-time increase of shocks-risk in ICD patients. A small percentage of these episodes (2-5%) are actually due to oversensing which may indicate imminent lead faiure.
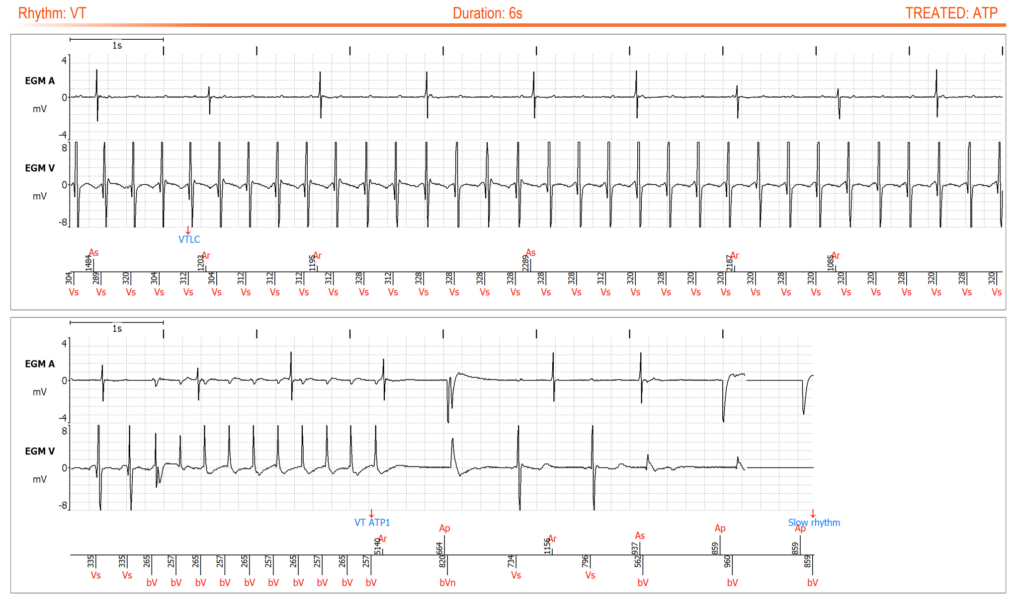
Alert “ATP DELIVERED” showing episode of ventricular tachycardia with correct detection and efficient treatment by ATP.
Alongside the detection of life-threatening arrhythmias, one of the main contributions of RM is early detection of atrial arrhythmias especially atrial fbrillation (AF), which expose patients to the risk of thromboembolic events, worsening of CHF, inappropriate ICD shocks, or loss of biventricular stimulation (in case of CRT patients). Recognizing AF is important to avoid inappropriate ICD therapies, since AF is responsible for the majority of them. The ECOST trial showed a 74% reduction in the number of inappropriate shock related to SVT in the RM arm compared to standard follow-up. With RM, physicians have the opportunity to initiate anticoagulation, where appropriate, and to optimize rate or rhythm control therapies preventing stroke- or AF-related CHF decompensation due to early detection of AF. A recent meta-analysis conducted in 16 randomized control trials of patients with CIEDs reported that RM, compared to in office follow-up, signifcantly reduced the risk of stroke, which may be due to the reduced time interval between AF onset and therapeutic intervention.
What about in-office follow-ups?
Although in-office visits for device checks serve an important purpose, prospective studies have shown that most in-office visits do not result in any significant reprogramming. While for patients with proper fonctioning pacemakers, most agree that in-office follow-up are no longer required, for ICDs it is much less clear. ICDs are inherently associated with the risk of inappropriate therapies, which can be a life threatening complication. For ICDs, device evaluation generally occurs every 3—6 months. With active remote monitoring, these visits may be performed less often, pushing the periods between in office check-ups to one year or beyond. As stated, the remote monitoring needs to be active, with observance of loss-of-transmissions and timely action on submitted alerts.