Guidelines
Lesson Materials
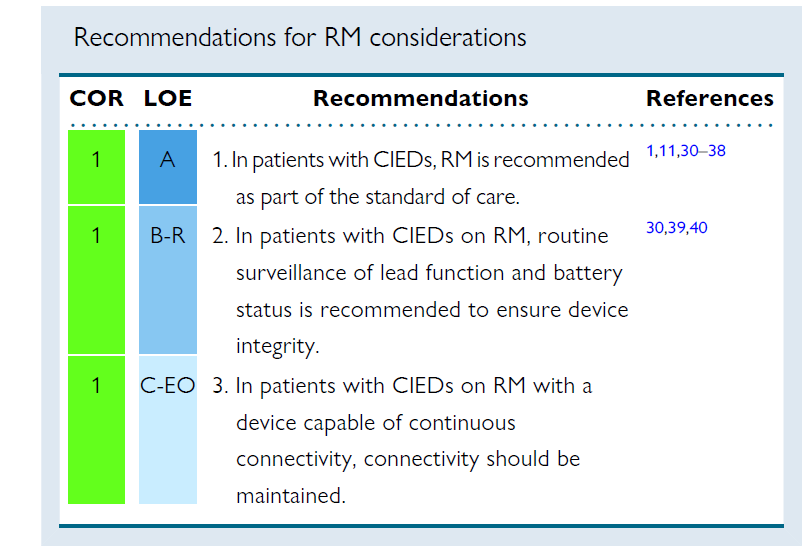
In patients with cardiac implantable electrical devices (CIED including PM, ICD and CRT), RM is recommended as standard of care in the 2015 and 2023 HRS/EHRA/APHRS/LAHRS Expert Consensus Statement on remote monitoring (RM). Several large, randomized studies as well as large registries and observational studies consistently demonstrated major organizational benefits, such as follow-up optimization, and clinical benefits, with improved patient management and clinical outcome associated with RM.
General benefits
RM reduces the number of health care visits and increases follow-up adherence and patient retention. It provides earlier detection of actionable events such as atrial and ventricular arrhythmias without compromising safety. It has been demonstrated to be useful in reducing inappropriate implantable cardioverter-defibrillator (ICD) shocks by early detection of atrial fibrillation (AF) with rapid ventricular response rates. T-wave oversensing, electromagnetic interference, and device malfunction. RM can facilitate early detection and quantification of AF episodes and arrhythmia burden that may prompt clinical reaction, preventing adverse events such as stroke, shock therapy, and HF. Continuous connectivity allows individualized patient treatment and continuous updating of therapeutic strategy.
RM is generally regarded as cost-effective, depending on the health care model and items assessed, as it results in reduction of in-hospital scheduled and emergency visits, reduction of diagnostic test burden, and reduction of follow-up duration and physician and nurse time. RM also reduces patient costs for travel to in-person visits, absence from work, and interruption of daily activities of patients and accompanying persons. Conflicting results do exist regarding the impact of RM on patient acceptance and quality of life. Several studies have reported a high rate of patient satisfaction for diverse aspects such as the patient’s perceived relationship with their health care providers, ease of use, psychological impact, and the ability to maintain follow-up compliance. Other studies observed neutral effects.
Device surveillance
RM allows effective and safe surveillance of device functioning with alerts for battery depletion, circuit disruption, and lead failure, ensuring device function and integrity. Early detection of malfunctions when the patient is still asymptomatic may prevent catastrophic consequences, particularly in cases of lead or device advisory. RM also allows for continuous connectivity of pacing thresholds, allowing optimization of battery longevity
Alert based remote monitoring
For patients with continuous connectivity, consistent connectivity depends on proper functioning of the RM home device as well as on telecommunication system availability and patient adherence to the follow-up plan. Many manufacturers currently provide mobile smartphone applications that can facilitate CIED RM transmission and alert patients to the status of RM connectivity, encouraging patient engagement and partnership vital to maintaining RM. Consistent connectivity is critical to maximize RM benefits by early detection of actionable events, allowing for early intervention for arrhythmias and HF decompensation, with potential to improve overall patient outcomes. Rapid response to implanted system technical failure as well as to changes in clinical status may impact patient outcomes.
Timing of remote monitoring enrollment
It can be beneficial to enroll patients with a CIED in an RM program within 2 weeks of CIED implantation, and ideally prior to hospital discharge if feasible. In a randomized trial comparing RM with conventional follow-up, enrollment in RM before discharge was associated with earlier detection of actionable events without increasing unnecessary in-patient evaluations. RM enrollment within 3 months of implant was associated with improved survival in all CIED types, but the survival benefit was greatest in patients with cardiac resynchronization therapy defibrillators (CRT-Ds).
Types of remote monitoring
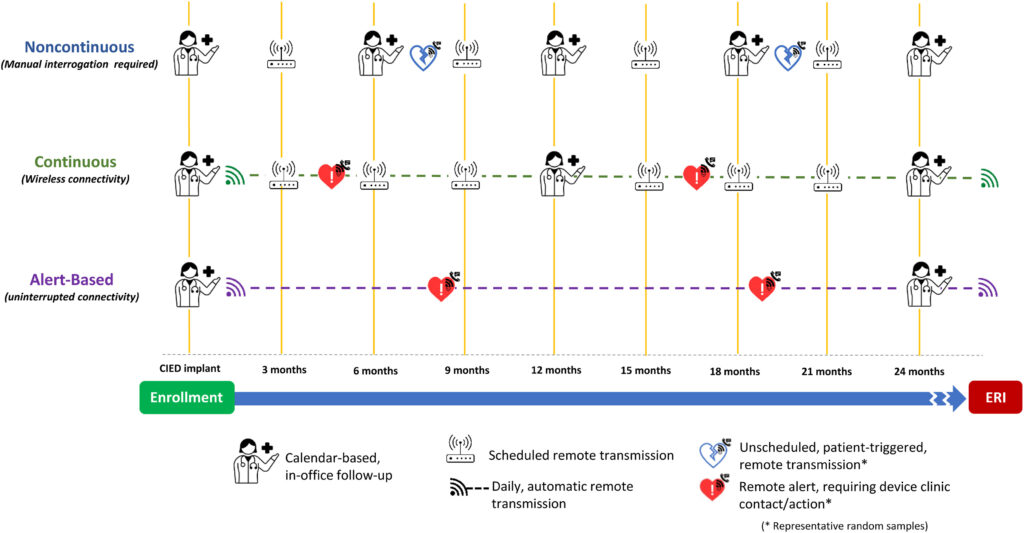
Remote device management may consist of multiple types of transmissions:
- Full remote device interrogation at scheduled intervals, mimics in-office visits.
- Automatic unscheduled RM transmission, consists of continuous connectivity with ongoing, real-time assessment of device function following predefined alert events.
- In the final type, patients can initiate a remote transmission when they experience an event.
Evidence regarding the frequency of remote follow-up interrogations and transmissions is lacking. In general, transmissions for ICDs should be more frequent than for PMs due to the increased complexity of their function as well as the in general, sicker population. There will be some circumstances (eg, if a patient is PM dependent) where the transmission frequency for PMs may match or exceed that for some ICDs. In most cases, a CRT-D could be treated like an ICD and a cardiac resynchronization therapy pacemaker (CRT-P) could be treated like a PM for RM follow-up.
The implementation of continuous connectivity extends remote patient management beyond periodic calendar-based follow-up. In randomized clinical trials, RM was associated with a reduction of hospital use and staff workload and a shorter time to clinical decisions. “Alert-based RM” was increasingly used during the COVID-19 pandemic out of necessity. The practice was effective and yielded a positive experience. This form of remote management has the potential to replace structured intermittent device follow-up (whether in-person or remote). This could minimize low-value effort, optimize clinic visits for actionable events, and decrease health care costs. For alert-based RM to be effective, there must be near-perfect connectivity, robust systems to assure connectivity from the manufacturers, and excellent patient compliance.
Alert types
The definition of high-priority alerts, and of the response to them, is crucial for organization of care pathways, prioritization of review of alerts, and definition of acceptable response timelines. A significant percentage, if not the majority, of alerts transmitted from remotely monitored CIED are nonactionable alerts (such as detection of known AF) and concern events that do not require immediate action. In contrast, and as demonstrated in randomized studies, reaction to alerts concerning battery capacity, lead integrity, and therapies delivered by ICDs for ventricular tachyarrhythmias has been shown to reduce adverse outcomes. Arrhythmic events such as shock therapies or ATP therapies delivered by the ICD not only indicate an increased risk for subsequent therapies, but may also indicate lead integrity issues. Reaction to these alerts may reduce adverse clinical events.
Handling alerts
Unscheduled alert transmissions and the associated workload are an ongoing concern for RM clinics. Alerts for arrhythmias that are already known, and where further alerts will not lead to any clinical action, can contribute to this workload.138 In an observational study, two-thirds of transmissions were reported to have shown at least one abnormal event, with the majority requiring no clinical action. Most nonactionable alerts occur for known arrhythmias. Individualizing RM alerts to suit patients’ individual clinical circumstances can improve clinic efficiency. Ideally, optimized alert programming would occur at the time of implantation based on individual clinical circumstances.Management of alerts is a crucial part of the workflow in each remote device clinic. Reactions to critical alerts and noncritical alerts need to be tailored to the individual patient. Reactions to alerts transmitted during nonbusiness hours are frequently a particular concern for RM clinics. Concerns include potential liability for nonimmediate response to incoming high-priority alerts. Nevertheless, there is no evidence for the need of an immediate response to alerts outside of the working hours. Most RM sites are not able to provide an immediate response. For this reason, it is crucial that patients and their care providers realize that RM should not be misinterpreted as a replacement for an emergency system.